What is Pontine Hemorrhage?
Pontine hemorrhages are a common form of intracerebral hemorrhage, and usually are a result of poorly controlled long-standing hypertension, although also have other causes. When due to chronic hypertension, the stigmata of chronic hypertensive encephalopathy are often present. It carries a very poor prognosis.
The pons is the largest component of the brain stem. When blood flow to the pons becomes interrupted, it causes a pontine stroke or pons stroke. When the disruption is caused by a blood clot in particular, it’s referred to as a pontine infarction or pontine infarct.
Epidemiology
Primary pontine hemorrhage accounts for ~7.5% (range 5-10%) of hemorrhagic strokes and has an incidence of ~3 per 100,000 people.
Cause of Pontine Stroke
Pontine strokes can be classified as either ischemic or hemorrhagic.
An ischemic stroke occurs when an artery in the brain becomes blocked by a blood clot, while a hemorrhagic stroke occurs when an artery in the brain bursts. Pontine strokes make up approximately 7% of all ischemic strokes (pontine infarct) and 10% of hemorrhagic strokes.
Hypertension and diabetes are two of the most common risk factors for all ischemic strokes and especially lacunar infarcts, a type of ischemic stroke that occurs in the deep areas of the brain such as the pons.
Other common causes of pontine stroke include diseases that affect the arteries such as small artery disease, large artery atherosclerosis (when the arteries become thickened with plaque), and cardiogenic emboli (when a blood clot travels from the heart to the brain).
Clinical Presentation of Pontine Hemorrhage
Patients present with sudden and precipitous neurological deficits. Depending on the speed at which the hematoma enlarges and the exact location, presentation may include:
- Decreased level of consciousness (most common)
- Long tract signs including quadriparesis
- Cranial nerve palsies
- Seizures
- Cheyne-Stokes respiration
- Pin-Point Pupil
- Dysarthria
- Dysphagia
- Locked-in syndrome: Involves paralysis of all four limbs (tetraplegia) as well as the face. The eyes are still able move. The survivor retains full cognitive function, aware of their environment but unable to interact with it except with eye movement — as long as the other areas of the pons that control eye movement were unaffected.
- Pure sensory deficits
Pathology
As is the case with penetrating arteries into the basal ganglia, the penetrating arteries from the basilar artery extending into the pons are subject to lipo-hyalinosis as a result of poorly-controlled hypertension. This renders the vessel wall prone to rupture. The larger paramedian perforators are more commonly the culprit vessels.
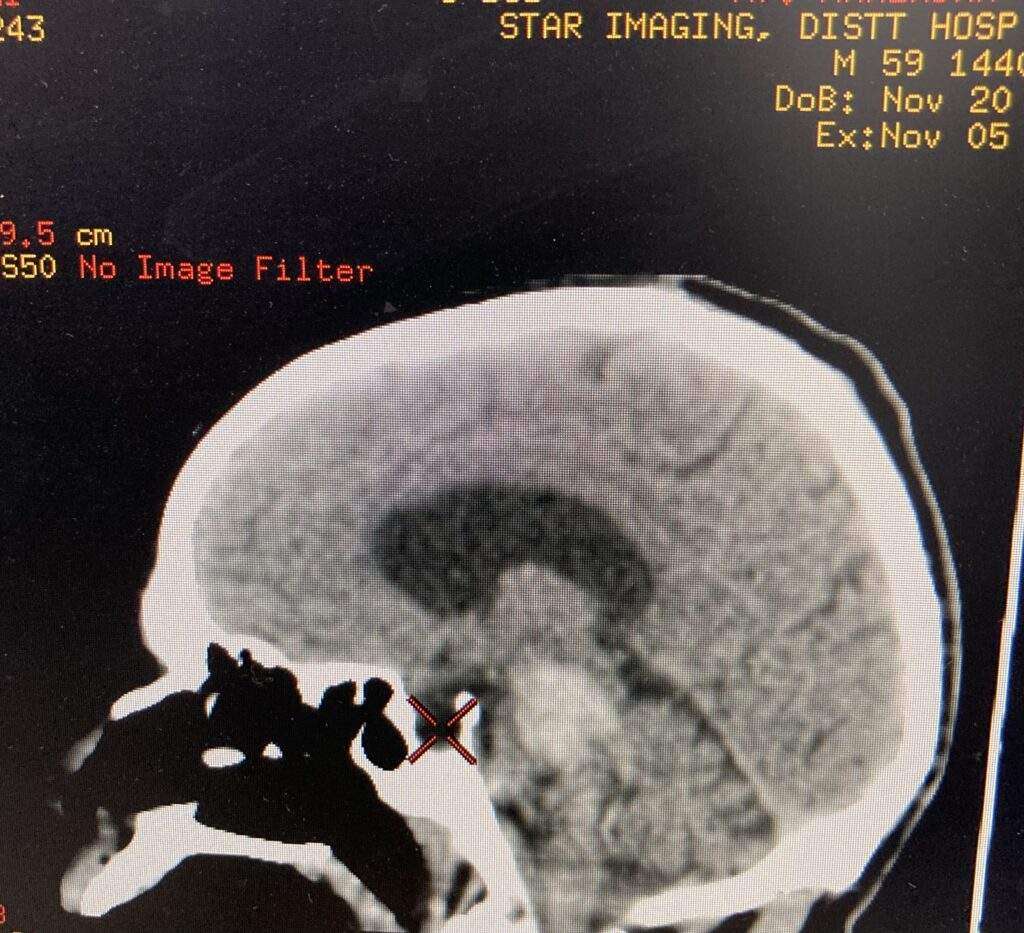
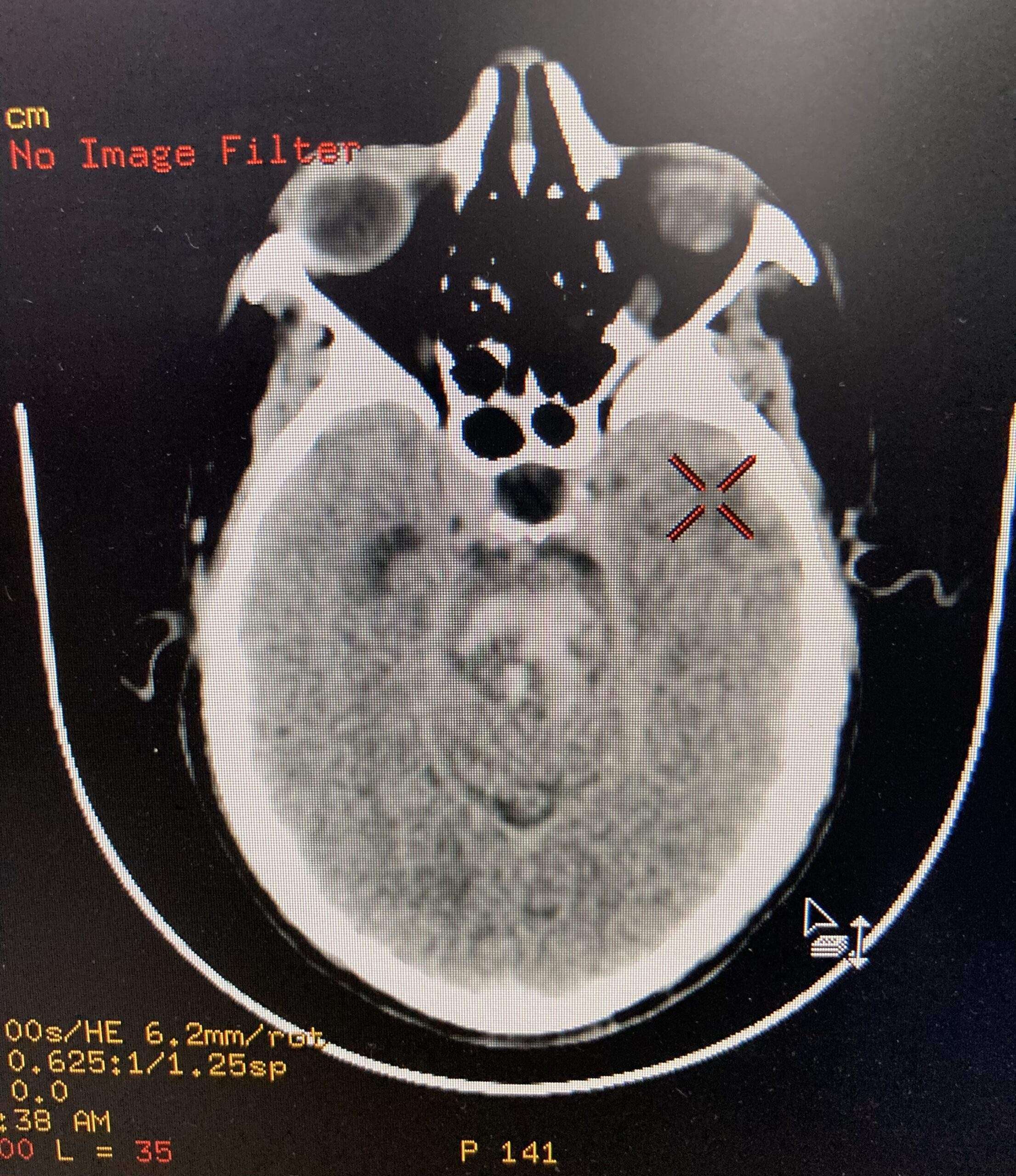
Radiographic features of Pontine Hemorrhage
CT
CT of the brain is usually the first, and often the only, investigation obtained upon presentation. Features typical of an acute intraparenchymal hemorrhage are noted, usually located centrally within the pons (on account of the larger paramedian perforators usually being the site of bleeding).
The hematoma more frequently extends in a rostro-caudal direction along the traversing long tracts rather than laterally into the middle cerebellar peduncle. Usually the hematoma does not extend beyond the pontomedullary junction inferiorly and the inferior midbrain superiorly. These hematomas frequently rupture into the 4th ventricle.
MRI
In patients who have small volume bleeds and who are thought to possibly have an underlying lesion, MRI may be of use (e.g. identification of a vascular malformation).
Treatment and Prognosis
Patient with this hemorrhages have a poor prognosis, with large bleeds being almost universally fatal. Open surgical evacuation of the clot is usually not performed, although stereotactic clot aspiration has been advocated by some.
In smaller hemorrhages, medical management and treatment of hydrocephalus with extraventricular drains may be life-saving, however, often with significant residual neurological deficits.
Overall mortality ranges between 30% and 90%, with the overall volume of the bleed and initial GCS being related to outcome.
Rehabilitation for Pontine Stroke Survivors
Rehabilitation can take many forms to address the unique secondary effects caused by a pontine stroke. Therapists will help you create a custom rehabilitation plan that addresses your unique goals to improve movement and/or sensation.
One major goal of rehabilitation is to spark neuroplasticity to help rewire the brain and recover as much function as possible. Neuroplasticity is activated through massed practice as the brain gets better at the activities and skills that we repeatedly practice.
Here are some of types of therapy that are commonly used to treat the effects of a pontine stroke:
Physical Therapy
During physical therapy, your therapist will guide you through rehabilitation exercises that help improve mobility in the affected muscles. Survivors with severe motor impairments can start slow with passive range of motion exercises to help prevent complications such as contractures or pressure sores. Passive movement also helps spark neuroplasticity and rewire the brain. Over time, they may be able to progress to more active exercises and even strengthening.
Occupational Therapy
Your occupational therapist specializes in maximizing independence with the activities of daily living. Your OT will provide you with both functional exercises and any necessary compensation techniques to help you complete your daily tasks. They can also offer recommendations for home modifications to help prevent falls, discuss safety concerns and precautions following sensation loss, and provide resources for getting back to work or back to drive again.
Speech Therapy
Speech therapists are able to address difficulties with speaking, swallowing, and general communication skills. They may use a variety of exercises to improve the strength and coordination of the muscles surrounding your mouth and face. They can also suggest methods of communication other than speaking, called augmentative and alternative communication (AAC). For example, if you have locked-in syndrome, they may recommend using technology designed to track your eye movements to communicate.
Home Therapy
A strong home exercise program after stroke can make a noticeable difference during recovery. Whether you have mild, moderate, or severe effects that you wish to recover, your therapist can provide suitable exercises for you to practice at home. Home therapy is essential to keep the brain constantly stimulated and maximize neuroplasticity.
Sensory Retraining
Sometimes a pontine stroke can cause changes in sensation such as numbness, tingling, or difficulty sensing temperature. For these sensory issues, sensory retraining exercises might be able to help. It involves safely exposing your skin to various textures and temperatures to stimulate the brain.
Recovery from Pontine Stroke
Overall, a pontine stroke can affect movement and/or sensation on one or both sides of the body. Although pontine infarcts are technically small in nature, they can create significant effects such as locked-in syndrome, especially when both sides of the pons were affected.
Fortunately, with a rigorous rehabilitation regimen, survivors can stimulate the brain and maximize their chances of recovery. Not all survivors will achieve a full recovery, but it’s a possibility for many. Approach your stroke recovery prognosis with curiosity to see how far you can go.